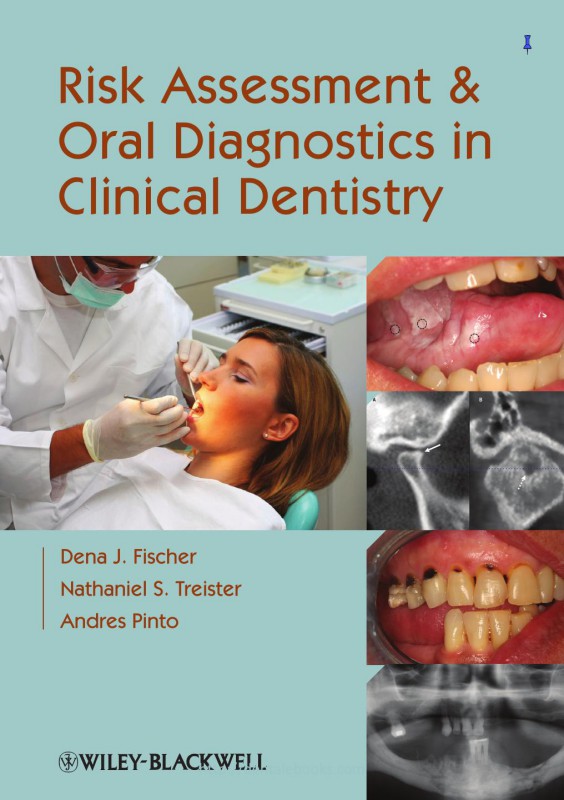
Risk Assessment and Oral Diagnostics in Clinical Dentistry 1st Edition by Dena Fischer, Nathaniel Treister, Andres Pinto ISBN 1118928954 9781118928950
$50.00 Original price was: $50.00.$25.00Current price is: $25.00.
Authors:Dena J. Fischer , Author sort:Fischer, Dena J. , Published:Published:Nov 2012
Risk Assessment and Oral Diagnostics in Clinical Dentistry 1st Edition by Dena Fischer, Nathaniel Treister, Andres Pinto – Ebook PDF Instant Download/Delivery. 1118928954, 9781118928950
Full download Risk Assessment and Oral Diagnostics in Clinical Dentistry 1st Edition after payment
Product details:
ISBN 10: 1118928954
ISBN 13: 9781118928950
Author: Dena Fischer, Nathaniel Treister, Andres Pinto
Risk Assessment and Oral Diagnostics in Clinical Dentistry aims to enable the dental practitioner to comfortably and capably assess when medical conditions may impact dental care and diagnose oral conditions using routine testing modalities.
Risk Assessment and Oral Diagnostics in Clinical Dentistry 1st Table of contents:
Part A Guidelines for Risk Assessment of Systemic Conditions that may Complicate or be Complicated by Dental Treatment
1 Basics of the Health History, Physical Examination, and Clinical Investigations
1.0 INTRODUCTION
1.1 Obtaining a complete medical history
1.1.1 Chief complaint
1.1.2 History of present illness
1.1.3 Past medical history
1.1.4 Medications and allergies
Table 1.1 Cytochrome P450-associated drug interactions.
1.1.5 Review of systems
Table 1.2 Potentially serious drug interactions that may interact with medications prescribed by oral health care providers.
1.1.6 Family and social history
1.1.7 Past dental history
1.2 Physical examination
Figure 1.1 62-year-old male with metastatic prostate cancer involving the clivus (affecting cranial nerves IX and XII on the right side) with progressive right-sided tongue and constrictor muscle weakness. Straight protrusion of the tongue (a) demonstrates right-sided muscle flaccidity, whereas excursion to the right side (b) demonstrates minimal movement.
1.2.1 Extraoral examination
Figure 1.2 68-year-old male with notable extraoral asymmetry and swelling (a), that upon intraoral examination (b), demonstrated a large poorly differentiated carcinoma of the right maxilla.
1.2.2 Intraoral examination
Figure 1.3 Well-defined area of leukoplakia of the anterior mandibular alveolar mucosa, with a distinct white appearance, against a background of normal-appearing pink mucosa.
Figure 1.4 Clear aqueous saliva expressed by palpating the parotid gland extraorally.
Figure 1.5 Squamous cell carcinoma of the right palatine tonsil (arrow), appearing enlarged and erythematous with extensive ulceration.
1.3 Ordering and performing laboratory tests
1.3.1 Basics of ordering laboratory tests
1.3.1.1 Identifying a clinical laboratory
1.3.1.2 Completion of forms
1.3.1.3 ICD-9 codes
1.3.2 Serologic studies
1.3.3 Microbiology studies
1.3.3.1 Performing cultures
1.3.3.2 Bacterial cultures
Figure 1.6 Persistent purulence despite broad-spectrum antibiotic therapy in a 50-year female with metastatic breast cancer and Stage 0 medication-associated osteonecrosis of the jaw.
1.3.3.3 Fungal cultures
1.3.3.4 Viral cultures
Figure 1.7 Viral culture kit.
1.3.3.5 Cytopathology studies
Figure 1.8 Cytology kit (a) and cytology specimen (b) demonstrating virally infected multinucleated cells, consistent with a diagnosis of herpes simplex virus infection.
Figure 1.9 Oral cytology specimen demonstrating Candida hyphae (linear organisms; solid arrow) and conidiae (ovoid budding organisms; broken arrow). Photomicrograph courtesy of Mark Lerman, DMD, Boston, MA.
1.3.4 Histopathology studies
1.3.4.1 Performing a biopsy
Figure 1.10 Large multifocal area of leukoplakia of the right lateral tongue in a patient already previously treated for oral squamous cell carcinoma. The three circles represent biopsy sites to obtain representative samples of the overall lesion.
Figure 1.11 Perilesional biopsy site marked by the dashed circle that is adjacent to, but not involving, an area of ulceration.
Figure 1.12 Punch biopsy sequence. The site of the biopsy is identified and the tissue punch is placed flat on the tissue (a); then the tissue punch is rotated back and forth with gentle downward pressure (b); and finally the tissue is secured with forceps, raised, and the deep base released with either scissors or a scalpel (c).
Figure 1.13 Excisional biopsy of a condyloma acuminatum of the posterior right soft palate (a, arrow). Following removal with a scalpel, silver nitrate (c) was applied to control hemostasis (b), leaving a black, cauterized wound (b).
1.3.4.2 Transport medium
1.3.4.3 Completion of the pathology requisition form
Figure 1.14 Typical pathology requisition form. In addition to the required information at the top of the page, the clinician should provide sufficient clinical details such as the size, location, and appearance of the lesion. Used with permission from Brigham and Women’s Hospital.
Table 1.3 Clinical descriptors of oral lesions.
1.3.4.4 Interpretation of pathology results
1.4 Radiology studies
1.4.1 Plain film
1.4.2 Computed tomography
Figure 1.15 Computed tomography of the mandible in a trauma patient. Axial view (a) demonstrates a symphisis fracture and the coronal view (b) demonstrates bilateral condylar head fractures.
1.4.3 Magnetic resonance imaging
Figure 1.16 Magnetic resonance imaging of the mandible in a patient with squamous cell carcinoma of the left posterior buccal vestibule demonstrating a large enhancing lesion (tumor, arrow) that does not appear to be invading into the alveolar bone.
1.4.4 Other imaging studies
Figure 1.17 Sialogram of the parotid gland demonstrating the ductal system with loss of normal acinar structures.
Figure 1.18 Positron emission tomography scan of the same patient from Figure 1.16, demonstrating the tumor in the left posterior mandible (arrow) as well as involvement of lymph nodes in the left neck (broken arrows).
Figure 1.19 Extensive area of leukoplakia in a patient that had previously undergone allogeneic hematopoietic cell transplantation. Photographs obtained at 6 (a) and 8 (b) years post-transplantation demonstrate clear progression of the lesion. Biopsies at both visits demonstrated hyperkeratosis only.
1.5 Suggested literature
2 Basic Tests and Evaluation Methods of Systemic Health
2.0 INTRODUCTION
2.1 Vital signs
Alert Box 2.1 Reference ranges for radial or carotid artery pulse.
Table 2.1 Classification of hypertension.*,†
2.2 Diagnostic fluids
2.2.1 Blood
2.2.2 Saliva as a diagnostic fluid
2.2.3 Other diagnostic fluids
2.3 General blood tests
Table 2.2 Complete blood count (CBC) tests.
Figure 2.1 Shorthand notation for common hematology values.
2.3.1 Hematopoiesis
2.3.2 Red blood cells
2.3.2.1 Basic tests of red blood cells
Alert Box 2.2 RBC value reference ranges and restrictions/modifications for dental treatment.
2.3.2.2 Red blood cell indices
Table 2.3 Classification of anemias.
2.3.2.3 Other RBC tests
2.3.2.4 Anemias
Figure 2.2 Pallor of the palate in a 41-year-old female with pernicious anemia.
Figure 2.3 Tongue pallor and loss of filiform papillae in a 36-year-old female with iron deficiency anemia.
2.3.2.4.1 Vitamin and mineral deficiencies
2.3.2.4.2 Hemolytic anemias
Figure 2.4 Localized soft tissue necrosis secondary to infarcts in a 38-year-old patient with sickle cell disease in sickle cell crisis.
2.3.2.4.3 Aplastic anemia
2.3.3 White blood cells
Alert Box 2.3 WBC Reference ranges and restrictions/modifications for dental treatment.*
2.4 Serum chemistry and electrolytes
Table 2.4 Reference ranges for serum chemistry, electrolyte, and vitamin/mineral values.
Figure 2.5 Shorthand notation for common chemistry values (Chem 7).
2.4.1 Liver function
Figure 2.6 Jaundice in the sclera of the eyes affecting a 65-year-old patient with acute hepatitis A.
2.4.2 Kidney function
Figure 2.7 Clinical (a) and radiographic (b) presentation of renal osteodystrophy in a patient with end-stage renal disease. Note the radiographic ground-glass trabecular pattern of bone.
2.4.3 Electrolytes
2.5 Suggested literature
3 Potential for Bleeding
3.0 INTRODUCTION
Figure 3.1 Multiple palatal petechiae and ecchymoses in a patient with severe thrombocytopenia secondary to aplastic anemia.
Figure 3.2 Petechiae of the marginal gingiva in a patient with severe thrombocytopenia secondary to acute leukemia.
Figure 3.3 Diffuse ecchymosis of the right buccal mucosa in an anticoagulated patient following an accidental fall.
Figure 3.4 Exophytic hematoma of the right buccal mucosa in a patient with severe thrombocytopenia associated with advanced multiple myeloma.
Figure 3.5 Persistent bleeding following a punch biopsy in a patient with previously undiagnosed Factor XI deficiency.
3.1 Platelets
Alert Box 3.1 Platelet count values and restrictions/modifications for dental treatment.*
3.1.1 Platelet tests
3.1.1.1 Platelet count
3.1.1.2 Bleeding time
3.1.1.3 Liver function tests
3.1.2 Platelet abnormalities
3.1.2.1 Medication-induced
Table 3.1 Medications administered in the outpatient setting that may increase the risk of oral bleeding.
3.1.2.1.1 Acetasylic acid and non-steroidal anti-inflammatory agents
3.1.2.1.2 ADP inhibitors
3.1.2.1.3 Chemotherapy agents
3.1.2.1.4 Other medications
3.1.2.2 Congenital
3.1.2.3 Acquired
Figure 3.6 Multiple hematomas of the lower labial mucosa in a patient with lupus-associated thrombocytopenia (a). The histopathology in (b) demonstrates sub- and intraepithelial collections of extravasated blood.
3.2 Coagulation
3.2.1 Tests of coagulation
Alert Box 3.2 Coagulation test values and restrictions/modifications for dental treatment.
3.2.1.1 aPTT
3.2.1.2 PT/INR
3.2.2 Coagulation abnormalities
3.2.2.1 Anticoagulant drugs
3.2.2.2 Coagulopathic conditions
3.2.2.2.1 Hemophilias
3.2.2.2.2 von Willebrand disease
3.2.2.2.3 Liver disease
3.2.3 Guidelines for dental treatment
3.2.3.1 General considerations
Table 3.2 Measures for management of post-operative oral bleeding.
3.2.3.2 Local measures
Figure 3.7 Use of Surgicel packed into a site of persistent subgingival bone bleeding following a crown-lengthening procedure in a patient with severe von Willebrand disease. Bleeding had persisted despite extensive prophylactic and post-operative systemic measures.
3.2.3.3 Medication-induced platelet disorders
3.2.3.4 Thrombocytopenia
3.2.3.5 Hemophilia A and B
Figure 3.8 Prolonged and uncontrolled gingival bleeding in a patient with advanced leukemia despite packing of Gelfoam (b). Gauze soaked in aminocaproic acid syrup was used locally for effective control of bleeding (c and d).
3.2.3.6 von Willebrand disease
3.2.3.7 Liver disease
3.3 Suggested literature
4 Potential for Infection
4.0 INTRODUCTION
4.1 Medical conditions associated with an increased risk of oral infection
4.1.1 Hematologic malignancies
Figure 4.1 Gingival infiltrate of leukemic cells in a 42-year-old female recently diagnosed with acute lymphocytic leukemia.
4.1.1.1 Leukemia
4.1.1.2 Lymphoma
4.1.1.3 Multiple myeloma
4.1.2 Aplastic anemia
4.1.3 HIV infection
Table 4.1 Oral manifestations of HIV disease.
Figure 4.2 Acute necrotizing ulcerative periodontitis in a 37-year-old AIDS patient with a CD4+ T-cell count of 2 cells/mm3.
Figure 4.3 Prominent nodular maxillary oral involvement in a 26-year-old male with advanced AIDS and multifocal disseminated Kaposi sarcoma.
Figure 4.4 Multiple nodular papillomas in a 46-year-old HIV-positive male who was noncompliant with antiretroviral therapy.
4.1.4 Endocrine disorders
4.2 Medications associated with an increased risk of infection
Table 4.2 Select medications associated with leukopenia.
4.2.1 Chemotherapy
4.2.2 Corticosteroid therapy and other immunomodulatory agents
4.3 Tests for evaluating infection risk
4.3.1 Basic tests of white blood cells
4.3.1.1 WBC differential count
Table 4.3 WBC differential values.
Figure 4.5 Gingival neutropenic ulceration in a young male being treated for acute myelogenous leukemia with profound neutropenia. Note the lack of marginal erythema, and note labial ulcerations and crusting consistent with recrudescent herpes simplex infection.
4.3.2 Adjunctive tests
4.4 Implications of abnormal wbc tests on provision of oral care
Alert Box 4.1 Absolute neutrophil count and infection risk.
4.5 Antibiotic prophylaxis for dental procedures
4.5.1 Cardiac complications
4.5.2 Prosthetic joint complications
4.5.3 Recommendations for antibiotic prophylaxis
Table 4.4 Indications for antibiotic prophylaxis prior to invasive dental procedures for the prevention of infective endocarditis.*,†
Table 4.5 Recommended antibiotics for the prevention of infective endocarditis in adults.*
4.6 Suggested literature
5 Potential for Poor Wound Healing
5.0 INTRODUCTION
Table 5.1 Risk assessment for poor wound healing.
5.1 Diabetes mellitus
Figure 5.1 Advanced periodontal disease in a 48-year-old male with poorly controlled diabetes mellitus who presented for evaluation of multiple loose teeth and halitosis.
5.1.1 Tests for diagnosis and monitoring of DM
Alert Box 5.1 Casual plasma glucose values in patients with diabetes mellitus.
5.1.1.1 Diagnosis of DM: Fasting plasma glucose and oral glucose tolerance tests
Table 5.2 Tests for diagnosis and monitoring of diabetes mellitus.
5.1.1.2 Glucose self-monitoring: Random plasma glucose
Figure 5.2 Home glucose meter for daily self-monitoring of random plasma glucose levels.
5.1.1.3 Diabetes control: Glycated hemoglobin (HbA1c)
Alert Box 5.2 Glycated hemoglobin values in patients with diabetes mellitus.
5.1.2 Implications of abnormal tests on dental care
5.2 Adrenal disorders
5.2.1 Tests of adrenal function
5.2.1.1 Cortisol
5.2.1.2 Aldosterone
5.2.1.3 Adrenocorticotropic hormone
5.2.2 Implications of abnormal tests on provision of oral care
Table 5.3 Cortisol equivalent of corticosteroid medications.
Table 5.4 Steroid supplementation guidelines prior to dental treatment.*,†
5.3 Bone metabolism
Figure 5.3 Delayed healing of an extraction socket in a patient with a history of radiation therapy for advanced squamous cell carcinoma of the right tonsil.
5.3.1 Bone metabolism tests
5.3.1.1 C-terminal telopeptide and N-terminal telopeptide
5.4 Other considerations
5.5 Suggested literature
Part B Guidelines for Diagnosis of Orofacial Conditions
6 Dental Caries and Periodontal Conditions
6.0 INTRODUCTION
6.1 Dental caries
6.1.1 Caries risk assessment
Table 6.1 Factors contributing to caries risk assessment.*
6.1.1.1 Caries risk groups
6.1.1.2 Plaque biofilms
6.1.1.3 Diet
6.1.1.4 Salivary function and buffering capacity
6.1.1.5 Microbial tests
6.1.2 Diagnosis of dental caries
Table 6.2 Classification of caries lesions in the International Caries Detection Assessment System (ICDAS).*
Table 6.3 Classification of dental caries.*
6.1.2.1 Clinical diagnostic modalities
Figure 6.1 World Health Organization periodontal probe.
Figure 6.2 Active smooth-surface caries lesions with loss of luster, whitish opaque enamel color, chalky surface texture (A), and localized surface defects (discontinuities, B).
Figure 6.3 (A) Active pit and fissure carious lesion with brownish-black color associated with surface defect and whitish opaque enamel surface with loss of luster; (B) inactive pit and fissure carious lesion with yellowish-brown color as well as smooth, intact surface and shiny appearance.
6.1.2.2 Radiographic diagnostic modalities
6.1.2.3 Classification and quantification of dental caries
Table 6.4 Definitions of early childhood caries.*
6.1.2.4 Other diagnostic modalities
6.2 Periodontal disease
Table 6.5 American Academy of Periodontology general categories of plaque-induced periodontal diseases from the International Workshop for Classification of Periodontal Diseases and Conditions.*
6.2.1 Risk factors for periodontal disease
6.2.1.1 Microbiologic testing for periodontal disease
6.2.2 Diagnosis of periodontal disease
6.2.2.1 Clinical diagnostic modalities
6.2.2.2 Radiographic diagnostic modalities
6.2.2.3 Classification of periodontal diseases
Table 6.6 Classification of periodontal diseases, modified from the International Workshop for Classification of Periodontal Diseases and Conditions.*
6.2.2.4 Other diagnostic modalities
6.3 Selected literature
7 Oral Infection
7.0 INTRODUCTION
7.1 Bacterial infection
7.1.1 Tests of bacterial infection
Table 7.1 Outline of oral infections, including etiology, clinical presentation, diagnosis, and management.
Figure 7.1 This patient with antiresorptive medication-associated jaw osteonecrosis developed a large abscess that was non-responsive to empiric antibiotic therapy. For aerobic culture, the purulent discharge is directly swabbed; however, for anaerobic culture, purulent material should be collected from within the abscess minimizing exposure to air.
7.1.2 Antimicrobials and spectrum
Table 7.2 Antibiotics commonly used in the management of odontogenic infections.
7.1.2.1 Topical therapy
7.1.2.2 Systemic therapy
7.2 Fungal infection
Figure 7.2 Pseudomembranous candidiasis of the buccal mucosa and soft palate in a patient on topical steroid therapy for management of oral lichen planus. Some of the white/yellow plaques are more confluent than others.
Figure 7.3 Erythematous candidiasis of the palate following the precise outline of the patient’s acrylic-based removable partial denture.
Figure 7.4 Angular cheilitis in a patient with Crohn disease with erythema and cracking of the corners of the mouth.
7.2.1 Tests of fungal infection
Table 7.3 Antifungal regimens for the management of oral candidiasis.
Figure 7.5 Persistent erythematous and pseudomembranous candidiasis despite high-dose fluconazole therapy in a patient on long-term immunosuppressive therapy. Culture and sensitivity demonstrated fluconazole resistance but voriconazole susceptibility.
Figure 7.6 Biopsy specimen of an erythematous tongue lesion from the same patient in Figure 7.5 following voriconazole therapy. Despite apparent clinical resolution of candidiasis, the PAS stain demonstrated evidence of continued fungal infection (filamentous rods in keratinized epithelium).
7.3 Viral infection
7.3.1 Tests of viral infection
7.3.2 Viral culture
Figure 7.7 Recrudescent HSV infection in an immunocompromised patient presenting with intact vesicles of the lips (a) and multiple shallow crop-like ulcerations of the hard palate (b). The intraoral lesions could be swabbed; however, the lip lesions would need to first be unroofed in order to obtain an adequate culture sample.
7.3.3 Viral cytology
7.3.4 Viral serology
Figure 7.8 Primary HSV infection that was initially believed to be recurrent herpes zoster infection due to the primarily unilateral distribution of lesions. Serology did not demonstrate anti-HSV IgM or IgG and viral culture confirmed HSV–1 positivity.
7.3.5 Biopsy
7.4 Factors that may contribute to infection
7.4.1 Immunosuppression
7.4.2 Salivary gland hypofunction
7.5 Selected literature
8 Salivary Conditions
8.0 INTRODUCTION
Table 8.1 Medications associated with xerostomia.
8.1 Implications of salivary hypofunction
8.1.1 Local infection
8.1.2 Dysphagia
8.1.3 Oral discomfort
8.1.4 Dysgeusia
Table 8.2 Medications associated with taste changes.
8.2 Diagnostic tests for saliva and salivary glands
8.2.1 Measurement of xerostomia and salivary hypofunction
Figure 8.1 Salivary flow collection procedures and measurement protocols.
Figure 8.2 Carlson-Crittenden collectors. Saliva drains gravimetrically to the bottom orifice (B) and through the collector to the adjacent tubing. The outer ring (A) is used to establish negative pressure on the buccal mucosa to maintain the collector in place.
8.2.2 Tests of salivary constituents
8.2.3 Salivary pH and buffering capacity
8.2.4 Imaging studies
8.2.4.1 Radiography
Figure 8.3 Occlusal film demonstrating a right submandibular gland sialolith in an asymptomatic 71-year-old female.
8.2.4.2 Ultrasonography
8.2.4.3 Scintigraphy
8.2.4.4 Magnetic resonance imaging
8.2.4.5 Sialoendoscopy
8.2.5 Other diagnostic modalities
8.3 Diagnosis of salivary gland disorders
8.3.1 Sialolithiasis
Figure 8.4 Sialolith causing salivary gland obstruction in a 63-year-old male complaining of acute pain in the left floor of the mouth. Note the positioning of the sialolith close to the duct orifice.
Figure 8.5 Purulent discharge from the left Stensen duct orifice in a 43-year-old male with a previous history of recurrent duct obstruction secondary to sialolithiasis.
8.3.2 Sialadenitis
8.3.3 Salivary gland infections
Figure 8.6 Acute parotid gland swelling in a 9-year-old female diagnosed with Sjögren syndrome, with an 18-month history of intermittent bilateral swelling and recurrent glandular infection.
8.3.4 Mucocele
Figure 8.7 Two mucoceles on the lower lip of a 14-year-old female with a history of factitious lip biting.
Figure 8.8 Ranula of the right sublingual gland in a 28-year-old male with a recent history of traumatic perforating injury to the floor of the mouth.
8.3.5 Necrotizing sialometaplasia
Figure 8.9 Necrotizing sialometaplasia that developed following administration of a local anesthetic block to the right palate of a 32-year-old female.
8.3.6 Sialadenosis
8.3.7 Sarcoidosis
8.4 Sjögren syndrome
Figure 8.10 16-year-old female diagnosed with Sjögren syndrome, presenting with severe hyposalivation, erythematous soft tissues, and rampant dental caries.
8.4.1 Diagnostic criteria
Table 8.3 European-American criteria for diagnosis of Sjögren syndrome.*,†
Table 8.4 Sjögren’s International Collaborative Clinical Alliance (SICCA) classification criteria for Sjögren syndrome.*
8.4.1.1 Oral signs and symptoms
8.4.1.2 Ocular signs and symptoms
8.4.1.3 Serology
Table 8.5 Serology for salivary gland disorders.
8.4.1.4 Minor salivary gland biopsy
8.5 Suggested literature
9 Oral Neoplastic Disease
9.0 INTRODUCTION
Table 9.1 Benign and malignant tumors of the head and neck.
Figure 9.1 57-year-old male with diffuse large B-cell lymphoma with acute onset of pain and paresthesia of the left posterior mandible and ramus. Axial T1-weighted MRI of the brain demonstrated unusual appearance of the marrow in the left mandible near the area of the inferior alveolar nerve foramen, with prolonged T1 and T2 signal, consistent with marrow infiltration of his underlying lymphoma.
Figure 9.2 62-year-old male with metastatic prostate cancer with progressive right-sided tongue and constrictor muscle weakness (patient is moving the tongue as far to the right as possible) and difficulty speaking and swallowing (a). Sagittal MRI (b) demonstrates the extent of the metastatic lesion in the area of the clivus. Axial images demonstrate narrowing of the outlet of the right cranial nerve XII (computed tomography; c), and cranial nerve IX (MRI; d).
Figure 9.3 Axial CT scan of a patient with advanced relapsed squamous cell carcinoma of the right mandible with destruction of the cortical bone.
Alert Box 9.1 Signs/symptoms suggestive of oral malignant disease.
9.1 Benign neoplasms of the oral cavity
9.2 Oral potentially malignant lesions
Figure 9.4 Proliferative verrucous leukoplakia of the left retromolar pad, mylohyoid ridge, and lateral tongue.
9.3 Oral squamous cell carcinoma
Figure 9.5 Squamous cell carcinomas of the oral cavity. (a) Ulceration and extensive erythematous changes of the left maxilla secondary to SCC arising from the maxillary sinus; (b) multifocal SCC of the facial gingiva and anterior buccal mucosa with an exophytic growth pattern; (c) recurrent SCC of the left ventrolateral tongue with a slightly exophytic ulcerative component and white changes; (d) ulcerative SCC of the left tonsil.
9.4 Other cancers of the oral cavity
Figure 9.6 Extranodal presentation of non-Hodgkin lymphoma with a large mass-like ulceration of the posterior right maxilla and associated tooth mobility and pain.
Figure 9.7 Gingival involvement in a patient with acute myelogenous leukemia, with sheet-like overgrowth and focal areas of hemorrhage.
9.5 Diagnostic tests
9.5.1 Physical examination
9.5.2 Tissue biopsy
Figure 9.8 Punch biopsy of the oral mucosa including normal histopathology (a) and the surgical specimen (b), demonstrating full thickness of epithelium (e) and connective tissue (c) Sufficient depth of the biopsy is necessary to assess for evidence of invasion beyond the basement membrane.
9.5.3 Cytology
9.5.4 Imaging studies
9.6 Adjunctive tests
9.6.1 Chemoluminescence and tissue reflectance
9.6.2 Autofluorescence
9.6.3 Toluidine blue/tolonium chloride
9.6.4 Oral brush cytology
9.6.5 Summary of recommendations for the use of adjunctive tests
9.7 Selected literature
10 Oral Complications Associated with Cancer Therapy
10.0 INTRODUCTION
Table 10.1 Early and late effects of cancer treatment.
10.1 Cancer pre-treatment risk assessment
Table 10.2 Risk assessment prior to cancer treatment.
Table 10.3 Potential causes of acute infection during cancer treatment.
10.1.1 Head and neck cancers
Alert Box 10.1 Prevention of oral treatment complications associated with surgical procedures that cause direct osseous Injury.
10.1.2 Hematologic malignancies
10.1.3 Antiresorptive therapy
10.2 Early effects of cancer treatment
10.2.1 Surgical procedures
10.2.2 Oral mucositis
Figure 10.1 Aphthous-like lesion on the left buccal mucosa of a patient on mTOR inhibitor therapy (targeted molecular cancer therapy) for sarcoma management.
Figure 10.2 Severe mucositis of the left lateral tongue in a patient undergoing chemotherapy and radiotherapy for squamous cell carcinoma of the left lateral tongue.
Figure 10.3 World Health Organization Oral Toxicity Scale.
Figure 10.4 National Cancer Institute (NCI) Common Toxicity Criteria for Adverse Events (CTCAE) version 4.0.
10.2.3 Oral infection
10.2.4 Acute graft-versus-host disease
Figure 10.5 55-year-old male at day 60 following allogeneic hematopoietic stem cell transplantation for chronic lymphocytic leukemia. The patient developed acute GVHD with erythema and desquamation of the skin, and oral manifestations included severe intraoral ulcerations with erythema and pseudomembrane formation.
10.3 Early/late effects of cancer treatment
10.3.1 Hyposalivation
10.3.2 Chronic GVHD
Figure 10.6 Chronic GVHD of the left buccal mucosa, presenting as an ulceration with pseudomembrane formation and surrounding erythema in the center of the lesion. Note the lichenoid appearance with reticular striae affecting the remainder of the buccal mucosa.
10.3.3 Neuropathic pain and neurotoxicity
10.3.4 Nutrition, taste, and smell impairment
10.4 Late effects of cancer treatment
10.4.1 Chronic mucosal changes
Figure 10.7 Fibrosis of the right buccal mucosa as a chronic mucosal change secondary to radiation therapy for oral squamous cell carcinoma.
10.4.2 Caries
Figure 10.8 Cervical dental caries primarily affecting the cervical portions of maxillary teeth in a patient who underwent radiation treatment for oral squamous cell carcinoma.
10.4.3 Post-radiation osteonecrosis
Figure 10.9 (a) Post-radiation osteonecrosis of the left mandible with exposed, necrotic bone; and (b) panoramic radiograph showing loss of cortical bone in the left mandible. Reprinted from Dental Clinics of North America 52(1), Fischer DJ and Epstein JB, Management of patients who have undergone head and neck cancer therapy,” pgs. 39–60, 2008, with permission from Elsevier.
10.4.4 Medication-associated osteonecrosis of the jaw
Figure 10.10 Medication-associated ONJ of the right mandible in a patient treated with antiresorptive therapy for management of bony metastases. Note the exposed, necrotic bone and secondary soft tissue infection.
Figure 10.11 Radiographic image illustrating an advanced case of medication-associated ONJ in a 70-year-old male with multiple myeloma on monthly zoledronic acid therapy. Dense sclerotic and mixed mottled (poorly defined radiolucent/radiopaque) changes are affecting the body of the mandible, and persistent extraction sockets are present in the right anterior mandible.
10.4.5 Trismus and other musculoskeletal presentations
Figure 10.12 10-year-old male post–allogeneic hematopoietic stem cell transplantation with a previous history of severe ulcerative oral chronic GVHD with subsequent peri- and intraoral fibrosis and trismus. This Dynasplint device was utilized to increase range of mandibular movement.
10.4.6 Dentofacial abnormalities
10.4.7 Recurrent disease, second primary cancers, and metastatic disease
10.5 Selected literature
11 Oral Manifestations of Autoimmune, Immune-Mediated, and Allergic Disorders
11.0 INTRODUCTION
11.1 Autoimmune conditions
11.1.1 Autoimmune conditions that target epithelium
11.1.1.1 Pemphigus vulgaris
Figure 11.1 Collapsed bulla in a 52-year-old female with pemphigus vulgaris.
Figure 11.2 Direct immunofluorescence pattern of a tissue specimen from a patient with pemphigus vulgaris.
11.1.1.2 Pemphigoid
Figure 11.3 Intact bulla on the left lateral tongue of 67-year-old female with mucous membrane pemphigoid complaining of persistent oral soreness.
Figure 11.4 Direct immunofluorescence pattern of a tissue specimen from a patient with mucous membrane pemphigoid.
11.1.2 Autoimmune conditions that target connective tissue
11.1.2.1 Lupus erythematosus
Figure 11.5 Malar rash on the cheeks of a 53-year-old female with systemic lupus erythematosus.
Table 11.1 American College of Rheumatology criteria for classification of systemic lupus erythematosus.*
Table 11.2 Clinical and laboratory findings of autoimmune, immune-mediated, and allergic conditions with oral manifestations.
Figure 11.6 Systemic lupus erythematosus lesion on the right buccal mucosa of a young female with an acute flare of symptoms. Note the central erosive presentation with radiating striae.
Table 11.3 Important serology values for rheumatologic disorders.
11.1.2.2 Systemic sclerosis
Figure 11.7 Sclerodactyly in a 52-year-old female with progressive systemic sclerosis who presented for consultation regarding facial pain and oral hygiene issues.
Figure 11.8 Significant mandibular angular notching/resorption in a patient with progressive systemic sclerosis affecting the facial skin.
11.1.2.3 Rheumatoid arthritis
Figure 11.9 Hand deformities in a female with chronic rheumatoid arthritis.
Figure 11.10 Bilateral condylar flattening in a 68-year-old female with rheumatoid arthritis and a maximal interincisal opening of 22 millimeters.
11.1.2.4 Mixed connective tissue disease
11.2 Immune-mediated conditions
11.2.1 Lichen planus
Figure 11.11 Cutaneous lichen planus of the lower leg in a 5-year-old female with concurrent extensive oral involvement. Note the fine striations that appear similar to the classic oral reticular lesions.
Figure 11.12 Reticular oral lichen planus on the left buccal mucosa of a 33-year-old female.
11.2.2 Lichenoid reactions
11.2.3 Recurrent aphthous stomatitis
Figure 11.13 Recurrent major aphthous stomatitis in the right soft palate and tonsillar pillar of a 24-year-old male.
11.2.4 Erythema multiforme
Figure 11.14 Erythema multiforme with lip crusting in a 28-year-old female.
11.2.5 Granulomatous conditions
11.2.5.1 Inflammatory bowel disease
Figure 11.15 Pyostomatitis vegetans in a 37-year-old male with an acute flare of ulcerative colitis complaining of gastrointestinal discomfort.
11.2.5.2 Orofacial granulomatosis
Figure 11.16 Crohn disease presenting as orofacial granulomatosis of the lips in a male with a 10-year history of the disease.
11.2.5.3 Wegener granulomatosis
Figure 11.17 Multiple gingival vegetative/granulomatous lesions in a 34-year-old female diagnosed with Wegener granulomatosis.
11.2.5.4 Sarcoidosis
11.3 Allergic disorders
Table 11.4 Types of allergic reactions.
11.3.1 Oral allergy syndrome
11.3.2 Contact hypersensitivity
Figure 11.18 Lichenoid response to a metal fixed partial denture on the lower left mandible in a 57-year-old female.
11.3.3 Plasma cell gingivitis
Figure 11.19 Plasma cell gingivitis on the maxillary arch of a young male. Note the brilliant erythematous appearance of the free and attached gingiva.
11.3.4 Angioedema
11.4 Suggested literature
12 Orofacial Pain Conditions
12.0 INTRODUCTION
Table 12.1 Categories of non-odontogenic orofacial pain conditions.
12.1 Pain mechanisms
Figure 12.1 Afferent pain pathway. The impulse follows the primary afferent neuron of V3 through the gasserian ganglion (GG) into the subnucleus caudalis region of the trigeminal spinal tract, where it synapses with a second-order neuron and travels through the neospinothalamic tract (NST Tract) or paleospinothalamic tract (PST Tract) to the thalamus and cortex. Reproduced with permission from Okeson JP. Bell’s Orofacial Pains, 5th ed., Figure 3.2, page 54, Quintessence Publishing Co. Inc., Chicago.
12.2 General classification of pain
Table 12.2 Characteristics of neuropathic pain.
12.3 Pain assessment
12.3.1 Pain history
Figure 12.2 Numeric rating scale.
12.3.2 Clinical pain assessment
12.3.3 Diagnostic imaging
Figure 12.3 T1-weighted MRI of the left temporomandibular joint. The jaw is closed, as indicated by the position of the condyle relative to the articular eminence. The articular disk, which is radiolucent (arrow), is in a normal position relative to the condyle.
Figure 12.4 T1-weighted MRI of the left temporomandibular joint. The jaw is in a closed position. The articular disk, which is radiolucent (arrow), is anteriorly displaced relative to the condyle.
12.3.4 Other diagnostic modalities
12.3.5 Behavioral aspects of pain
Figure 12.5 Graded Chronic Pain Scale and Assessment. Reference: von Korff M, Ormal J, Dworkin SF. Grading the severity of chronic pain. Pain 1992;15:133–149.
12.4 Classification and diagnosis of pain conditions
12.4.1 Temporomandibular disorders
Table 12.3 Diagnostic categories of temporomandibular disorders.
Figure 12.6 Cone beam computed tomography (CBCT) of the temporomandibular joints. (a) Degenerative joint changes of the right TMJ with flattening of the glenoid fossa, osteophytic growth at the anterior margin of the head of the condyle, and anterior lipping of the condyle (solid arrow); (b) the right TMJ shows degenerative joint changes signified by widening of the glenoid fossa, sclerosis of the roof of the glenoid fossa, and osteophyte formation at the anterior margin of the condylar head. The well-circumscribed, homogeneous radiolucency is a subchondral bone “cyst” (broken arrow) that corresponds to an area of osseous degeneration that typically contains fibrous and/or granulation tissue. Figures courtesy of Dr. Richard Monahan, University of Illinois at Chicago.
12.4.2 Neuropathic pain
Alert Box 12.1 Signs of elevated suspicion for a craniofacial tumor or lesion.
12.4.2.1 Episodic neuropathic pain
12.4.2.2 Continuous neuropathic pain
12.4.3 Other pain conditions
12.4.3.1 Burning mouth syndrome
12.4.3.2 Giant cell arteritis
12.4.3.3 Atypical facial pain
12.4.3.4 Sympathetically maintained pain
12.4.3.5 Headache
12.5 Selected literature
People also search for Risk Assessment and Oral Diagnostics in Clinical Dentistry 1st:
risk assessment and oral diagnostics in clinical dentistry
dental clinical audit examples
what is risk assessment in dentistry
what should an assessment for oral health include
what is clinical audit in dentistry