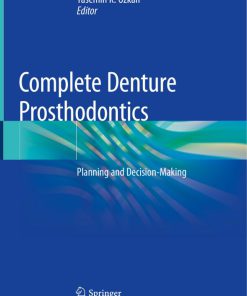
Planning and Making Crowns and Bridges 4th Edition by Bernard Smith, Leslie Howe 0415398509 9780415398503
$50.00 Original price was: $50.00.$25.00Current price is: $25.00.
Authors:Bernard G. N. Smith; Leslie C. Howe , Series:Dentistry [328] , Tags:Medical; General; Dentistry; Oral Surgery; Dermatology , Author sort:Smith, Bernard G. N. & Howe, Leslie C. , Ids:Google; 9780203090633 , Languages:Languages:eng , Published:Published:Oct 2013 , Publisher:CRC Press , Comments:Comments:This highly successful text, which has achieved wide acclaim among practitioners and is a recommended text in the major dental schools, has again been revised and updated to keep it at the forefront of clinical practice. As before, the intention is to help solve real clinical problems by guiding dentists to make the right initial decision and then
Planning and Making Crowns and Bridges 4th Edition by Bernard Smith, Leslie Howe – Ebook PDF Instant Download/Delivery. 0415398509, 9780415398503
Full download Planning and Making Crowns and Bridges 4th Edition after payment
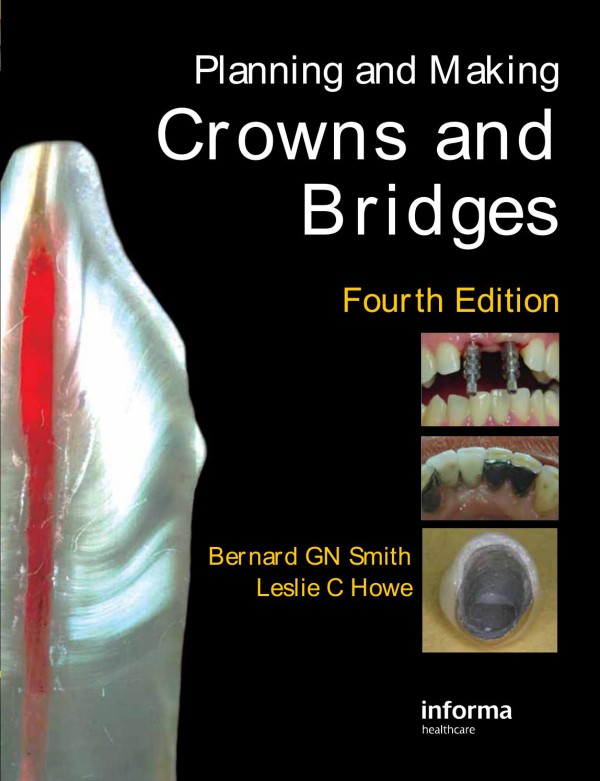
Product details:
ISBN 10: 0415398509
ISBN 13: 9780415398503
Author: Bernard G.N. Smith; Leslie C. Howe
This highly successful text, which has achieved wide acclaim among practitioners and is a recommended text in the major dental schools, has again been revised and updated to keep it at the forefront of clinical practice.
Planning and Making Crowns and Bridges 4th Table of contents:
Part 1 Crowns
1 Indications and contraindications for crowns
General indications and contraindications for crowns
Crowns versus fillings in the treatment of caries
General indications for crowns for other reasons
Badly broken-down teeth
Primary trauma
Tooth wear
Hypoplastic conditions
To alter the shape, size or inclination of teeth
To alter the occlusion
As part of another restoration
Combined indications
Multiple crowns
Appearance
Function
Mechanical problems
Indications for anterior crowns
Caries and trauma
Non-vital teeth
Tooth wear
Hypoplastic conditions
As part of other restorations
What are the alternatives to anterior crowns?
Internal and external bleaching
Internal bleaching
External bleaching
Composite restorations
Composite and porcelain veneers
Appearance
Reversibility
Cost
Surveys of success and failures of veneers
Physical properties
An alternative to porcelain veneers –resin bonded ceramic crowns
Restoration of badly broken-down teeth
Restoration of root-filled teeth
As part of another restoration
What are the alternatives to posterior crowns?
Bonded or pin-retained amalgam restorations
Tooth-coloured posterior restorations
Gold inlays and onlays protecting weak cusps
Ceramic inlays and onlays
Choosing the right posterior restoration
2 Types of crown
Anterior complete crowns for vital teeth
Ceramic crowns
Traditional porcelain jacket crowns (PJCs)
Pressed ceramic crowns
Laboratory milled cores and crowns
Zirconia cores
Chair-side milled restorations
Cast ceramic systems
Reinforced porcelains
Thin ceramic resin bonded crowns (see also Chapter l)
Choosing between ceramic crowns
Advantages
Disadvantages
Metal–ceramic crowns (Figure 2.1k and l)
Advantages
Disadvantages
Other types of anterior complete crowns
Cast metal acrylic or composite faced crowns
Fibre-reinforced composite crowns
Anterior crowns for root-filled teeth
Composite (or glass ionomer) core and crown
Post and core and separate crown
Post shapes
Comparisons of post shapes
Parallel: smooth or serrated (Figure 2.5b and c)
Tapered: smooth or serrated
Parallel: threaded
Tapered-threaded (Figure 2.5d right)
Choosing between post systems
One-piece post crown
Other types of crown for root-filled teeth
Posterior complete crowns
Cast metal crowns
Metal–ceramic crowns
Ceramic crowns
Posterior partial crowns
‘Three-quarter’ crowns
Other types of posterior partial crowns
Cores for posterior crowns
Cores of amalgam, composite or glass ionomer cement
Cast posterior cores
3 Designing crown preparations
The principles of crown preparation design
Related to materials
Metal crowns
Ceramic crowns
Metal–ceramic materials
Related to function
Occlusion
Future wear
Related to appearance
Labial, buccal, incisal and proximal reduction
Occlusal reduction of posterior teeth
Crown margins
Related to adjacent teeth
Clearance to avoid damage to adjacent teeth
Path of insertion
Oral hygiene and technical considerations
Related to periodontal tissues
Related to the pulp
Retention
Mechanical retention
‘Adhesive’ retention
Retention for conventional crowns
Retention against vertical loss
Interlocking minor undercuts
Taper of the preparation
Length of the preparation
Retention against other displacing forces
Avoiding failure from other causes
Fracture or distortion of tooth tissue
Fracture of ceramic crowns
Distortion of metal
Casting difficulties
Designing specific crown preparations
Posterior complete crown preparations
All-metal crowns
Metal–ceramic crowns
Anterior crown preparations: crowns for vital teeth
Ceramic crowns
Metal–ceramic crowns
Post-retained crowns
Posterior partial crown preparation
4 Occlusal considerations
A functional approach to occlusion
The functional compared with the orthodontic approach
Fixed compared with removable prosthetic approaches
Mandibular movements and definition of terms
Terminal hinge axis (THA) and the retruded arc of movement (or closure)
Intercuspal position (ICP)
Retruded contact position (RCP)
Mandibular movements
Retrusive movements
Protrusive excursion
Left and right lateral excursions
Occlusal interferences and occlusal harmony
Occlusal interferences
Occlusal harmony
‘Premature contact’
Occlusal stability (not the same as harmony)
Occlusal vertical dimension (OVD)
Creating interocclusal space for teeth to be crowned
Temporomandibular dysfunction (TMD)
Examination and analysis of the occlusion
Clinical examination of the occlusion
Clinical aids
Articulating paper or foil
Wax
Occlusal registration silicones
Plastic strips
Study casts
Articulated study casts
Occlusal adjustments prior to tooth preparation
Occlusal objectives in making crowns and bridges
Clinical and laboratory management of the occlusion
Avoiding loss of occlusal relationships
Maintaining occlusal relationships with temporary restorations
Recording the occlusion
Hand-held models
Simple-hinge articulator (Figure 4.11)
Semi-adjustable articulator (see Figures 4.10 and 4.12)
Fully adjustable articulator
Laboratory stages
Trimming the casts
Articulating the casts
Shaping the occlusal surfaces
Adjusting the occlusion of restorations in the mouth before cementation
Occlusal marking materials
Adjusting in intercuspal position
Adjustments in lateral, protrusive and retrusive excursions
Stability
Adjustment techniques
5 Planning and making crowns
History and examination
Considering the whole patient
Patient attitude and informed consent
Age
Sex
Social history
Cost
Considering the whole mouth
Oral hygiene
Condition of the remaining teeth
Considering the individual tooth
The value of the tooth
Appearance (Figure 5.2)
Condition of the crown of the tooth, the pulp and periodontium
Occlusion
Root length
Decisions to be made
Is the tooth to be kept or extracted?
If the tooth is to be kept, is it to be restored by a crown or a filling?
If the tooth is to be crowned, is any preparatory treatment necessary?
Detailed planning of the crown
Appearance
Shade
Clinical modifications
Assessing the remaining tooth structure and its environment
The need for a core
The choice of the type of crown and the material
Detailed design of the preparation
Planning and executing the clinical and laboratory stages
Appointments
Clinical and laboratory stages
6 Clinical techniques for making crowns
Planning stages before preparing the tooth
Study casts and opposing cast
Photographs
Planning the tooth preparation
Planning the appearance
Diagnostic wax-ups
Shade
Technique for shade selection
Planning the impression
Making a special tray (Figure 6.4)
Planning the temporary crown
Preformed temporary crowns
Chair-side temporary crowns
Laboratory temporary crowns
Building up the core
Managing worn, short teeth
Tooth preparation
Choice of instruments
Stages in the preparation
Preparing teeth for complete posterior crowns
Occlusal reduction
Axial reduction
Buccal and lingual surfaces
Mesial and distal surfaces
Margins
Finishing
Preparing teeth for complete anterior crowns
Incisal and proximal reduction
Labial reduction
Gingival-palatal reduction
Incisal-palatal reduction
Finishing
Preparing anterior teeth for post crowns
Post hole preparation
Removing the root canal filling
Shaping the post hole
Finishing the preparation
Temporary crowns
Preformed temporary crowns
Polycarbonate temporary crowns
Stainless-steel temporary crowns
Aluminium crown forms
Chair-side techniques for making temporary crowns
Injection or pouring techniques
Moulding techniques
Temporary post crown techniques
Differences between temporary and provisional crowns
Laboratory-made provisional restorations
Cementation of temporary and provisional crowns
The working impression
Impression materials (Figure 6.21)
Silicone impression materials
Polyether impression material
Reversible hydrocolloid
Impression techniques
Single material technique (e.g. polyether)
Two viscosity material technique (e.g. light- and heavy-body silicone)
Putty and wash (e.g. silicone)
Polymer materials and gloves
Gingival retraction
Compressed air (Figure 6.23a and b)
Kaolin pastes (Figure 6.23c, d and e)
Cord and impregnated cord (Figure 6.23d)
Electrosurgery (Figures 6.14a and 6.20a)
Occlusal records
Silicone occlusal records
Wax occlusal records
Removing temporary crowns
Trying in the permanent crown
Safety precautions
The checking procedure
Checking and adjusting the fit
Checking retention
Checking and adjusting contact points and axial contours
Checking and adjusting the shade
Checking and adjusting the occlusion
Cementation
Choice of cements
Zinc phosphate cement
Resin-based and adhesive cements
Glass ionomer cements
Cementation technique
Preparing the crown
Preparing the tooth
Mixing and applying the cement
Inserting the crown
Oral hygiene instruction and maintenance by the patient
Recall, assessment, maintenance and repair
Assessment
Oral hygiene
Margins
Structure of the crown
Appearance
Radiographs
Adjustments and repairs to crowns in situ
Part 2 Bridges
7 Indications for bridges compared with partial dentures and implant-retained prostheses
General terminology
General advantages and disadvantages of replacing missing teeth
Advantages of replacing missing teeth
Appearance
Ability to eat
Occlusal stability
Other advantages
Disadvantages of replacing missing teeth
Damage to tooth and pulp
Secondary caries
Failures
How long do bridges last?
Effects on the periodontium
Cost and discomfort
The choice between fixed and removable prostheses
General considerations
Patient attitude
Age and sex
Confidence
Occupation
General health
Appearance
General dental considerations
Local dental considerations
Examples of specific indications for bridges, dentures and implant bridges
Scope of this book
8 Types of bridge
Conventional and minimum-preparation bridges
Basic designs, combinations and variations
The four basic designs (Figure 8.1)
Fixed–fixed bridge
Fixed–movable bridge
Cantilever bridge
Spring cantilever bridge
Combination designs
Hybrid design
Variations
Removable bridges
Advantages and disadvantages of the four basic designs
Choice of materials
Metal only
Metal–ceramic
Ceramic only
Combinations of materials
Types of minimum-preparation bridge
Advantages of minimum-preparation bridges in general
Disadvantages of minimum-preparation bridges in general
9 Components of bridges: retainers, pontics and connectors
Retainers
Major or minor
Complete crown (full crown), partial crown, intracoronal or minimum-preparation retainers?
Materials
Criteria for choosing a suitable retainer
Appearance
The condition of the abutment tooth
Conservation of tooth tissue
Alignment of abutment teeth and retention
Occlusion
Cost
Pontics
Principles of design
Cleansability
Appearance
Strength
The surfaces of a pontic
The ridge surface
Wash-through (Figure 9.4a)
Dome-shaped (Figure 9.4b and c)
Ridge-lap and modified ridge-lap (Figure 9.4d, e and f)
Saddle
The effects of pontics on the ridge
The occlusal surface
The approximal surfaces
The buccal and lingual surfaces
Materials
Connectors
Fixed connectors
Movable connectors
10 Designing and planning bridges
Criteria for selecting a bridge design
Support
Conservation of tooth tissue
Cleansability
Appearance
Planning bridges
Collecting information about the patient
Consideration of the whole patient
Clinical examination
Assessing abutment teeth
Length of span
Occlusion
Shape of ridge
Predicting the final result
Study casts
Intra-oral trials
Partial dentures
Other reversible intra-oral modifications
Temporary and provisional bridges
Practical steps in choosing a bridge design
General approach
Details of stages in the design process
Selecting abutment teeth
Selecting the retainers
Selecting the pontics and connectors
Planning the occlusion
Examples of the bridge design process
11 Clinical techniques for bridge construction
Preoperative procedures
Occlusal adjustment
Preparations for a temporary bridge
Preparing the abutment teeth
Preparations for minimum-preparation bridges
Preparations for conventional bridges
Paralleling techniques for conventional preparations
Paralleling by eye
Extra-oral survey
Paralleling devices for crown preparations
Making temporary and provisional bridges
Choice of material
Choice of technique
Chair-side construction
Laboratory-made provisional bridges
Cementing temporary and provisional bridges
The working impression
Occlusal records
Trying in the metal framework or separate units
Localization techniques
Try-in and trial cementation of finished bridges
Permanent cementation
Minimum-preparation bridges
Summary of clinical techniques for minimum-preparation bridges
First appointment
Laboratory stage
Second appointment
Success with minimum preparation bridges
The cementation of conventional bridges
Oral hygiene instructions and maintenance
Part 3 Implants, splints and maintenance
12 Dental implants
The purpose of this chapter
Basic principles
Osseo-integration
General indications for implants
General contraindications to implants
Choosing between implants and bridges
Designs of dental implants
Abutments
Screw- versus cement-retained
Restorations
Implant survival
Planning
Implant numbers and position
Lack of bone and grafting
Appearance
Radiographs
Surgical stent
Provisional restorations
Surgical procedures
One stage
Two stage
Immediate placement/restoration
Restorative procedures
Abutment choice
Impressions
Placing the restoration
Maintenance
Complications
13 Fixed splints
Indications for fixed splints
Trauma
Periodontal disease
Orthodontic retention
Cleft palate
Additional retention
Short-term, intermediate and permanent splints
Short-term splints
Intermediate-term splints
Permanent splints
Fixed splints compared with removable splints
Types of short-term, intermediate and permanent fixed splint
Examples of short-term splints
Acid-etch retained composite splints (Figure 13.3)
Wire and composite splint (Figure I3.4)
Examples of intermediate- and long-term splints
Fibre-reinforced splint (Figure I3.5a)
Flexi-wire splints (Figure I3. 5b)
Cast metal intermediate and permanent minimum-preparation splints
Complete-crown splints
Intracoronal splints
The appearance of anterior splints
Selecting an anterior splint
Clinical techniques for permanent splints
Tooth preparation for complete-crown splints
Temporary splints
Impressions
Cementation
14 Crown and bridge failures and repairs
General considerations of success and failure and the value of survey data
How long will it last?
There are difficulties in defining failure
How long do crowns and conventional bridges last?
How long do minimum-preparation bridges last?
How long do porcelain veneers and inlays last?
How long do implants last?
How long have modern restorations been available?
A rough guide for advice to patients, to be modified by knowledge of the patient’s specific circumstances
Causes of failure and some solutions
Loss of retention
Conventional fixed–fixed bridges and splinted retainers
Minimum-preparation bridges
Other bridges
Solutions for loss of retention
Mechanical failure of crowns or bridge components
Porcelain fracture
Failure of connectors: soldered and laser welded
Avoiding soldered or welded joints in the first place
Distortion
Occlusal wear and perforation
Lost acrylic facings
Changes in the abutment tooth
Periodontal disease
Problems with the pulp
Caries
Fracture of the prepared natural crown or root
Movement of the tooth
Design failures
Abutment preparation design
Inadequate bridge design
Under–prescribed bridges
Over-prescribed bridges
Inadequate clinical or laboratory technique
Marginal deficiencies
Positive ledge (overhang)
Negative ledge
Defect
Poor shape or colour
Occlusal problems
Techniques for adjustments, adaptations and repairs to crowns and bridges
Assessing the seriousness of the problem
Adjustments by grinding and polishing in situ
Repairs in situ
Occlusal repairs
Repairs at the margins
Repairs to porcelain
Repairs by removing or replacing parts of a bridge
Replacing lost facings
Removing and/or replacing entire sections of a bridge
Removing abutment teeth
Extending bridges
Removing crowns and bridges
People also search for Planning and Making Crowns and Bridges 4th:
2 crowns and a bridge cost
7 bridges marketing
7 bridges of konigsberg activity
7 bridges answer