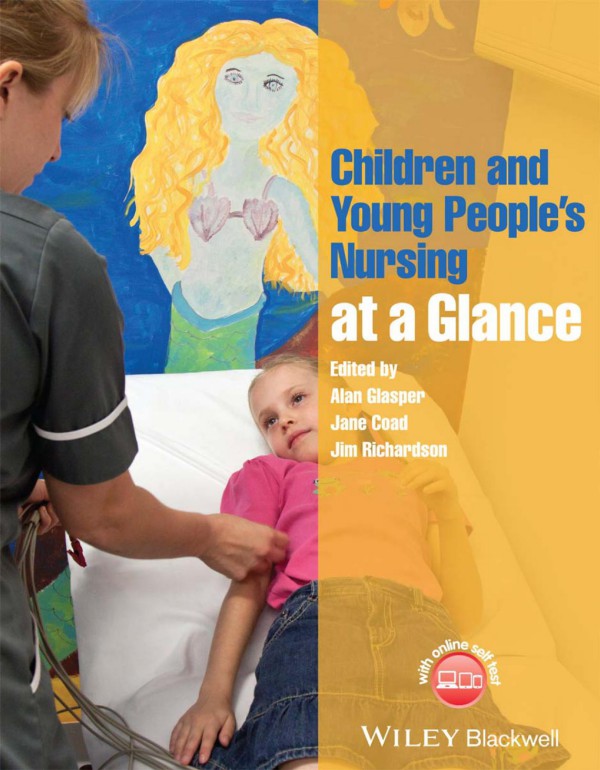
Children and Young Peoples Nursing at a Glance 1st Edition by Alan Glasper, Jane Coad, Jim Richardson 1118516281 9781118516287
$50.00 Original price was: $50.00.$25.00Current price is: $25.00.
Authors:Alan Glasper , Author sort:Glasper, Alan , Published:Published:Oct 2014
Children and Young Peoples Nursing at a Glance 1st Edition by Alan Glasper, Jane Coad, Jim Richardson – Ebook PDF Instant Download/Delivery. 1118516281, 9781118516287
Full download Children and Young Peoples Nursing at a Glance 1st Edition after payment
Product details:
ISBN 10: 1118516281
ISBN 13: 9781118516287
Author: Alan Glasper; Jane Coad; Jim Richardson
Children and Young People’s Nursing at a Glance, is the perfect companion for study and revision for pre-registration children’s nursing students from the publishers of the market-leading at a Glance series. Divided into seven sections it explores assessment and screening, working with families, the newborn infant, the developing child, child health policy, nursing the sick child and young person and chronic and life-limiting conditions.
This comprehensive book is an invaluable resource for pre-registration nursing students as well as newly qualified nurses wanting to consolidate and expand their knowledge of children and young people’s nursing.
- Breaks down complex aspects of child health care in an accessible and un-intimidating way
- The perfect revision and consolidation textbook
- Linked closely with the NMC standards for pre-registration nursing education, and the essential skills clusters framework
- Highly visual colour presentation, with approximately 130 illustrations
- Includes boxes, summary boxes, key points and recommendations for practice to improve the learning experience
- Supported by a companion website featuring over 500 interactive multiple choice questions (www.ataglanceseries.com/nursing/children)
- Available in a range of digital formats – perfect for ‘on the go’ study and revision
Children and Young Peoples Nursing at a Glance 1st Table of contents:
Part 1: Assessment and screening
1 Assessment of the child
Interviewing – history taking
Observation – subjective data
Measuring – objective data
Summary
2 SBAR framework
Inter-professional working
Communication barriers
When using SBAR tool the practitioner should aim to:
3 The nursing process
What is nursing theory?
What is the nursing process?
Planning care
Summary
4 Nursing models
Nursing models used in children and young people’s nursing
How nursing models can be used in practice
Summary
5 The care plan
Assessment
What to assess
Planning
Implementation
Evaluation
Documentation
6 Record keeping
What constitutes a patient record?
CIA mnemonic
Ensuring good record keeping
What colour ink should nurses use when making records?
All nurses should follow the no ELBOW rule when making notes
Problems faced by nurses in keeping records
How long should records for children be kept?
Summary
7 Engagement and participation of children and young people
What are the practical hints and tips that can assist in achieving effective engagement and participation of children and young people?
What to avoid
8 Observation of the well child
9 Observation of the sick child
Introduction
The importance of observation
Child, young person and family-centred care
10 Septic screening
What is sepsis?
Stabilization of the infant or child
Blood tests
Urine
Stool sample
Chest X-ray
Lumbar puncture for CSF sample
Swabs
Consent
11 Advanced physical assessment
Airway
Breathing
Circulation
Disability
Exposure
12 Developmental assessment
Assessment
Genetics and nature versus nurture
Developmental milestones
Developmental delay
Implications for practice
13 Paediatric Early Warning Score
Calculating the Paediatric Early Warning Score
Limitations
14 Paediatric critical care
Recognition and management of the seriously ill child
15 Understanding investigations
Radiology
Sampling of cerebrospinal fluid
Blood samples
Sputum samples
Gastric washings
Nasopharyngeal aspirate
Per nasal swabs
Urine samples
Biopsy
16 Understanding blood gas analysis
pH
Buffers
Respiration
Base deficit
Renal tubular secretion
Anion gap
Sampling
17 Understanding blood chemistry
Electrolytes
Kidney function
Liver function
Acid–base balance
18 Understanding pathology specimen collection
Important principles when collecting specimens
Obtaining blood samples
Urine collection
Stool specimens
Transporting specimens
19 Understanding X-rays
How do X-rays work?
What is radiation?
The importance of staying still
Other types of imaging
20 Pulse oximetry
The pulse oximeter
The pulse oximeter probe
Indications for use and clinical application
Limitations of pulse oximetry
21 Central venous devices
Types of CVAD
Accessing CVADs
Care of CVADs
Complications
22 Tracheostomy care
Stoma and skin care
Suctioning
Humidification
Tube changes
Safety
Communication
Feeding
Complications
23 Infant resuscitation
Unresponsive – shout for help!
Open airway
Not breathing normally?
Rescue breaths
24 Young person resuscitation
Safe to approach
Stimulate
Shout
Airway
Breathing
Circulation
Definitive care
25 Resuscitation drugs
Adrenaline
Amiodarone
Atropine
Adenosine
Glucose
26 Emergency care
Nursing competency
The unwell baby
Common presentations in preschool children
Common presentations in school-aged children
Common presentations in adolescents
Safeguarding
Part 2: Working with families
27 Partnership
Effective partnership
Partnership and the multidisciplinary team
Parental stress and partnership
Mothers and fathers
Parental needs
Communication
28 Family centred care
What is family?
Models that facilitate a family centred approach to care
Advantages of family centred care
Challenges of family centred care
Summary
29 Family health promotion
What is important to the family?
Challenges to family health promotion
30 Communicating with children
Factors influencing communication
31 Hospital play
What constitutes hospital play?
Effects of a hospital admission
Role of the hospital play specialist
Stages of hospital preparation
32 Role of the community children’s nurse
Prevalence of chronic illness in childhood
Benefits of home care for children with a chronic illness
Role of the community children’s nurse
33 Collaboration with schools
34 Family information leaflets
Writing patient information leaflets
Consider the content and style of the leaflet
Use the 10 principles of clear writing
Consider the order of the information in your leaflet
Producing the leaflet
35 Safeguarding
From Maria Colwell (1973) to Peter Connolly (2007)
Munro Report
36 Fabricated or induced illness
37 Gaining consent or assent
38 Clinical holding
Considerations
Pre-holding considerations
Care during clinical holding
Post-holding considerations
39 Breaking bad or significant news
Preparing to break bad news
Supporting the family when bad news is given
After the bad news has been broken
40 Care of the dying child
Quality care for the dying child and family
Physical needs
Psychosocial needs
Spiritual needs
41 Dealing with aggression
What is aggression?
What causes aggression?
Emotional or impulsive aggression
Triggers of aggression
De-escalating physical aggression
42 Minimizing the effects of hospitalization
The experience of hospitalization
Interventions and adverse experiences of hospital
Interventions to alleviate the impact of hospitalization
43 Transition
Challenges to transitioning to home
Assessing needs for discharge to home
Specific needs
Integrated care pathway
Part 3: The newborn infant
44 Fetal development
Pre-embryonic development
Embryonic development
Fetal development
Fetal circulation
Adaptation at birth
45 Neonatal examination
46 Neonatal screening tests
Neonatal screening programmes
Sample collection and analysis
Conditions commonly screened
47 The premature baby
Causes of prematurity
Outcome
48 Neonatal transport
Planning a transport
49 Jaundice and hyperbilirubinaemia
Physiology of bilirubin
Hyperbilirubinaemia
Causes
Investigations of jaundice
Management of jaundice
Phototherapy
Care of a baby having phototherapy
50 Congenital heart disease
Pathophysiology
Diagnosis
Common conditions
Management of cardiac disease
Follow-up and prognosis
51 Neonatal resuscitation
Preparation and readiness
Keep infants warm: avoid heat loss
Initial assessment at birth
Follow ABC approach
Drugs
Babies needing specialist neonatal care
Parents, communication, record keeping
52 Incubator/Babytherm care
Heat balance
Heat loss
Four mechanisms of heat transfer
Incubator and Babytherm management and care
Weaning from an incubator or Babytherm
53 Sudden infant death syndrome
Definition
Incidence
Measures in place to reduce the risk
Advice to parents to help reduce the risks
Smoking
Part 4: The developing child
54 Nutrition in childhood
Importance of good nutritional assessment
Nutrition in the under-fives
Nutrition in school aged children
Nutrition in young people aged 12+
55 Breastfeeding
56 Bottle feeding
Types of infant formula
Preparing infant formula
57 Feed calculations
58 Percentile charts
Definition
Background
Potential triggers
59 Child development: 0–5 years
60 Child development: 5–16 years
61 Age-appropriate behaviours
Growth
Development
Age-inappropriate behaviours
62 Common behavioural problems of childhood
Common emotional and behavioural problems
Crying babies and colic
Feeding problems
Sleeping problems
Temper tantrums
Unwanted or aggressive behaviour
63 Adolescent development
Physical development
Brain development and changes in cognition (thinking)
Identity
Changing social relationships
Young people as service users
64 Child health promotion
What is child health promotion?
Do children’s nurses need to promote health?
Involving children
Ethics
Evaluation
Where is health promoted to children?
65 Immunity and immunization
Immunity
How immunizations work
Population immunity
Safe immunization
Immunization controversies
66 Childhood immunizations
Immunizations given at 2, 3 and 4 months
Immunizations given at 12–13 months
Immunizations given at 3 years 4 months or soon after
Immunizations given to girls at 12–13 years
Immunizations given to teenagers aged 13–18 years
Other immunzations available
Common problems
Treatment
When not to immunize
Part 5: Child heath policy
67 Child health policy
68 The rights of children in hospital
69 The NHS Change Model
Application of the NHS Change Model to innovation in children’s services
70 Young person policy
How can the ‘You’re Welcome’ criteria help nurses improve health care for young people?
How can nurses self-review their compliance to the ‘You’re Welcome’ standards?
71 Child disability policy
Part 6: Nursing the sick child and young person
72 Pain assessment
Self-report tools
Behavioural cues
Physiological cues
73 Pain management
Why managing pain in children is important
Summary of current guidelines
What does pain management involve?
Pharmacological interventions
Physical and psychological interventions
74 Preoperative preparation
Preadmission clinic
Hospital admission
Effects of hospitalization
Informed consent
Patient safety and risk management
Fasting guidelines
75 Postoperative care
Community perspective
76 Pressure area care
Categories of pressure ulcers
77 Managing fluid balance
Distribution of body fluids
Mechanisms of fluid balance
Management of the child with fluid imbalance
Oral fluid requirements
Intravenous fluid requirements
78 Administering medication
Contemporary issues
Involving the child, young person and family
Medicines safety
Calculation formula
Units of measurement
Calculating IV fluid rates
79 Drug calculations
Numeracy
Nursing and Midwifery Council
Skills
Estimation
Using a calculator
Checking the dose
Recommendations for practice
80 Enteral and nasogastric feeding
Enteral feeding
Nasogastric feeding
Orogastric feeding
Gastrostomy feeding
81 The feverish child
Fever
Thermoregulation
Physiology
Clinical assessment
Management
82 Infectious childhood diseases
83 Assessing infectious diseases
What is infectious disease?
Infectious agents
Epidemiology
Portal of entry
Source
Symptomatology
Disease course
Site of infection
Virulence factors
Treatment and protection
84 Prevention of infection
Context and definition
Prevention and control of infection
Specific pathogens
Actions to control transmission of infections
Hand hygiene
85 Hyponatraemia and its prevention
Movement of body fluid and electrolytes
Sodium
What is hyponatraemia?
Management of the child with hyponatraemia
Preventing hyponatraemia
86 Thermal injuries
Incidence
Priorities (Figure 86.1)
Total body surface area
Assessment tools
Burns
Compartment syndrome
Scalds
87 Childhood fractures
Types of closed fractures
The healing process
Management
Complications
88 Plaster care
Reasons for application
Preparation of the child
Applying the cast
Potential problems
89 Traction care
What is traction?
Why is traction used?
Types of traction
Care of the traction
General care considerations
90 Neurovascular observations
Compartment syndrome
Neurovascular observations
Further considerations of neurovascular observations
91 Neurological problems
Cerebral palsy
Headache
Stroke
Seizures
Neuromuscular or neuropathic conditions
92 Brain injury and coma
Physiology
Coma
93 Seizures
Causes of seizures
Epilepsy
Nursing care
Further investigations
Treatment
Follow-up care
94 Meningitis
Common causes
Prevention
Assessment
Planning care
Diagnosis
Management of bacterial meningitis
Potential complications
95 Septicaemia
Definition
Other terms
Management principles
Maximize oxygen delivery
Reduce oxygen demand
Optimize cardiac output
General considerations
96 Respiratory problems
Respiratory assessment
Bronchiolitis
Upper airway obstruction
Respiratory infections
Common respiratory interventions
97 Asthma
Asthma
Psychosocial impact of asthma
Role of Asthma UK
Treatment and management
Review
Emergency management
98 CPAP and BiPAP
Respiratory failure
Continuous positive airway pressure and bi-level positive airway pressure
Further considerations
99 Cardiovascular assessment and shock
Cardiac output
100 Inflammatory bowel disease
IBD and children
Diagnostic tools
Considerations for children and families diagnosed with IBD
101 Gastro-oesophageal reflux
What is reflux?
What causes reflux?
How is reflux diagnosed?
Treatments for GOR and GORD
Do infants grow out of GOR?
102 Coeliac disease
What causes coeliac disease?
Who should be tested for coeliac disease?
How is coeliac disease diagnosed?
How is coeliac disease treated?
103 Appendicitis
Principles of care
Preoperative care
Postoperative care
104 Constipation
The constipated child
Management of the child with functional constipation and faecal impaction
Drugs used in constipation
Disimpaction
Patient education
Maintenance therapy
105 Renal problems
Kidney function in children
Kidney structure
Structural renal disorders
Acquired renal disorders in childhood
Renal tract infection
Acute renal injury (failure)
End-stage renal damage (chronic renal failure)
Renal replacement therapy
Kidney transplantation
Tumours
Renal injury
Tests used in renal disorders
106 Haematological problems
Easy bruising
Petechial rash
Thrombocytopenia with absent radii (TAR)
Fanconi’s anaemia
Purpura fulminans
Hermansky–Pudlack syndrome
Haemophilia
Dactylitis
Facial appearance in β-thalassaemia major
107 Musculoskeletal problems
Developmental dysplasia of the hip
Congenital talipes equinovarus
Scoliosis
Slipped upper femoral epiphysis
Perthes’ disease
108 Reproductive and sexual problems
Structural abnormalities
Developmental issues
109 Skin conditions
Assessing the child with a rash
110 Atopic eczema
Diagnosis
Assessment
Part 7: Chronic and life-limiting conditions
111 Living with chronic illness
Definitions
Impact on the child and family
Child and young person first and foremost
112 Cystic fibrosis management
Detection of CF
Common problems and management
Impact on family
113 Juvenile idiopathic arthritis
Management
114 Epilepsy
Seizures
Generalized seizures
Partial seizures
Treatment
Status epilepticus
115 Childhood cancer
Nurse as supporter
Nurse as physical care provider
Nurse as teacher and educator
Nurse as team player
Summary
116 Cleft lip and palate
Cleft services
Support and management
Common problems and their management
Syndromes
Reparative surgery for lip and palate
Postoperative care
117 Diabetes
Complications and associated conditions
Treatment
Psychological and social issues
118 Diabetes management
Insulin regimens
Insulin types
Insulin administration
Nutrition
Physical activity
Illness management
119 Childhood obesity
Causes of childhood obesity
Current statistics
National Child Measurement Programme
Health risks
What can be done?
Change4Life
120 Eating disorders
What are eating disorders?
Who is affected by eating disorders?
Causes of eating disorders
Treatment
121 Mental health problems
What is a mental health problem?
Types of services
Types of mental health problems
Recognizing problems
122 Self-harm in childhood
What is self-harm?
What causes self-harming behaviour?
Management and treatment
123 What is a learning disability?
124 Autistic spectrum disorder
What is autistic spectrum disorder?
Autism
Causes
Brain differences
Triad of impairment
Supporting children with ASD
125 Communicating with the child who has a learning disability
126 Positive behavioural support
What is positive behavioural support?
127 Atrioventricular septal defect in children with learning disability
Symptoms
Treatment
Follow-up advice
128 Genetic conditions: Down’s syndrome
Genetics
Phenotype features
Diagnosis
Specific medical problems in Down’s syndrome
Prognosis
129 Other genetic conditions
Phenylketonuria
Duchenne muscular dystrophy
References and further reading
People also search for Children and Young Peoples Nursing at a Glance 1st:
children’s hospital nursing program
children’s nurse practitioner jobs
children’s nursing specialties inc
how to work in pediatric nursing